Home
Productos Populares
-
¡Oferta!

Bandoleras | Moraleja – Bandolera de piel# marrón | Pedro Miralles Mujer
€ 137.76€ 64.78 Añadir al carrito -
¡Oferta!

Sandalias Tacón | Aprilia – Sandalias de tacón destalonada de piel metalizada# beige/47-talla-35 | Pedro Miralles Mujer
€ 122.51€ 67.24 Seleccionar opciones -
¡Oferta!

Zapato Plano | Adelaide – Bailarinas planas destalonadas de piel# beige/47-talla-35 | Pedro Miralles Mujer
€ 122.26€ 57.40 Seleccionar opciones -
¡Oferta!

Sandalias Planas | Soria negro | Pedro Miralles Mujer
€ 147.93€ 66.42 Seleccionar opciones
Últimos Productos
-
¡Oferta!

Zapato Plano | Adelaide – Bailarinas planas destalonadas de piel# nude | Pedro Miralles Mujer
€ 161.95€ 63.96 Seleccionar opciones -
¡Oferta!
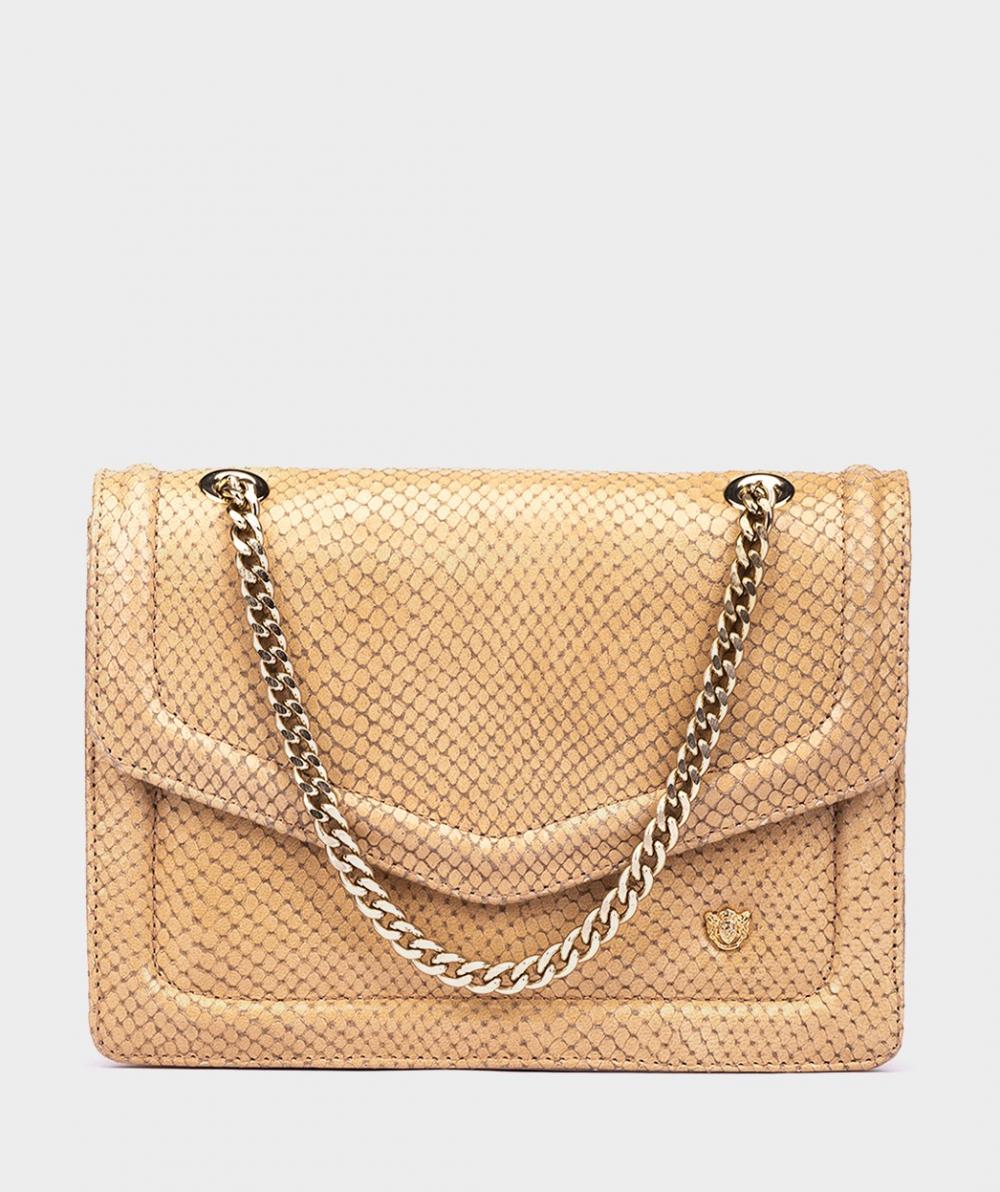
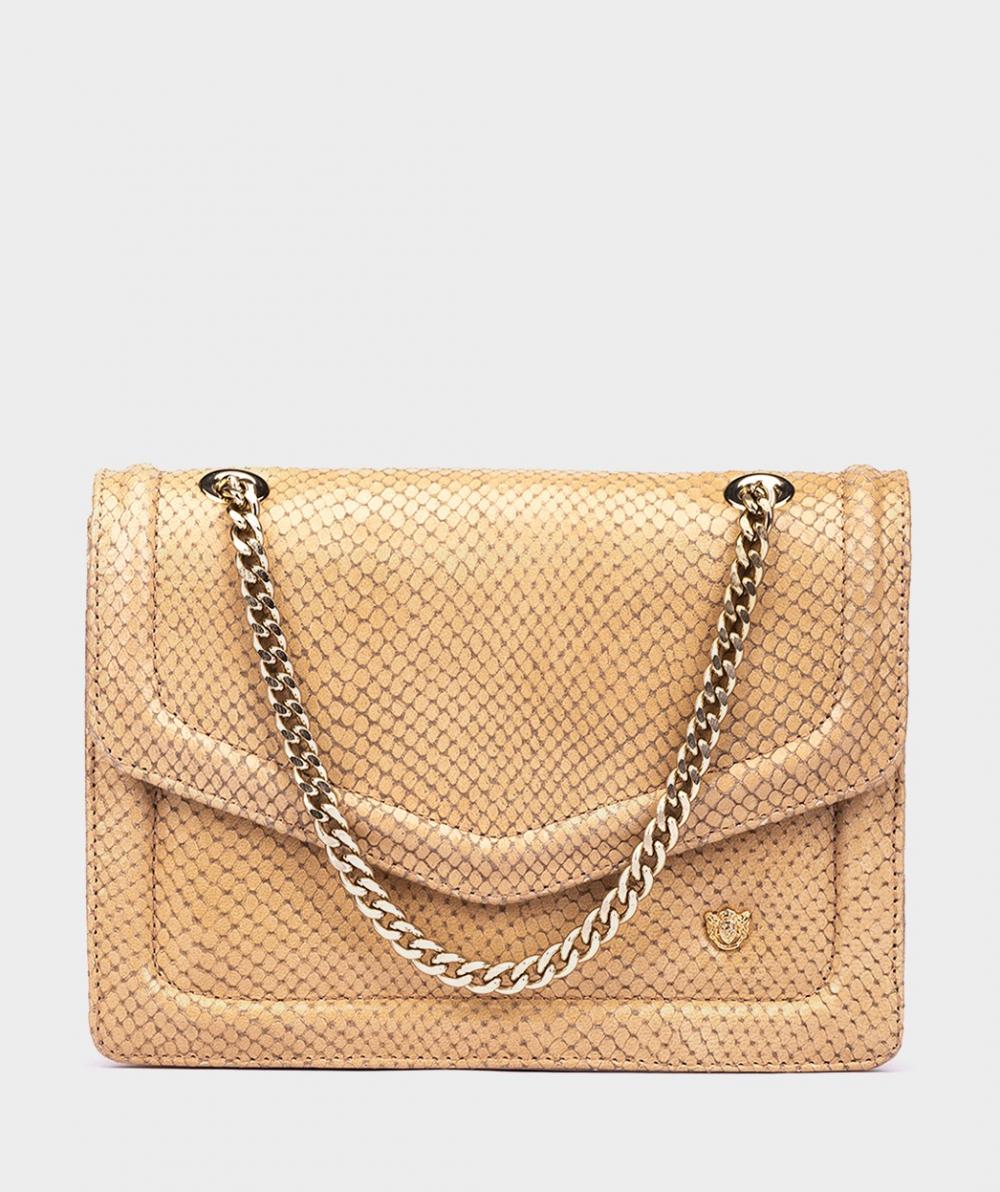
Bolsos De Hombro | Luzzi – Bolso de hombro de piel efecto cocodrilo# beige/133-talla-u | Pedro Miralles Mujer
€ 104.55€ 68.88 Añadir al carrito -
¡Oferta!

Botas | Springfield – Bota de media caña de piel de serraje.# marrón | Pedro Miralles Mujer
€ 159.90€ 63.14 Seleccionar opciones -
¡Oferta!

Sandalias Planas | Guadalupe – Sandalias planas de piel# azul | Pedro Miralles Mujer
€ 93.48€ 61.50 Seleccionar opciones